
It is normal for our brains to shrink as we age but abnormal to lose basic cognitive function or brain cells in large numbers. Alzheimer’s disease kills our brain cells, known as neurons, leading to thinking and memory decline. Overtime, affected individuals will gradually lose their ability to live independently. Over 5 million Americans have Alzheimer’s disease, 65,000 of those individuals reside in Oregon with another 110,000 in Washington. Between 2017 and 2018 there was a $20 billion rise in total care spent for individuals suffering from Alzheimer’s disease. It is becoming increasingly clear that better treatments are needed now more than ever.
Naturally occurring amyloid protein collect between neurons to form plaques. Abnormally folded tau protein forms neurofibrillary tangles inside neurons blocking their transport system and preventing communication with other neurons. When neurons are damaged connections between neural networks degrade causing brain regions to shrink, or atrophy (see Figure 1 showing brain shrinkage over a one year period in a patient with early disease). The brain areas most affected are responsible for memory, as the disease progresses it continues to affect other regions essential for language, reasoning, and more.
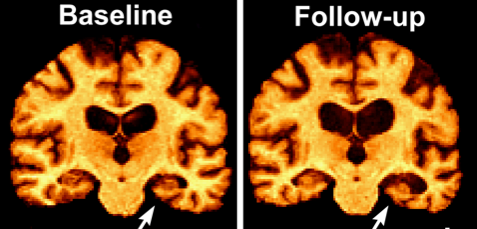
Figure 1. MRI scans of patient with MCI at baseline and 1 year later in follow-up; arrows point to the memory circuit called the hippocampus which has rapidly atrophied.
The disease can be divided into three stages. The first stage is called preclinical Alzheimer’s disease where subtle cognitive changes occur and often go unnoticed. The second stage–prodromal Alzheimer’s disease–or mild cognitive impairment (MCI), is when memory problems become obvious to family members, but the affected person can still live alone. The last stage is called Alzheimer’s disease dementia, where the individual’s ability to perform independent activities of daily living is impaired.
An Alzheimer’s diagnosis is confirmed by clinical interpretation and biomarker identification by measuring amyloid in the cerebral spinal fluid or with Amyloid-PET (Positron Emission Tomography) scans. These scans make it possible for us to view the amyloid plaques and, with Tau-PET, the tangles within the brain; allowing us to identify individuals at risk for the disease even before symptoms arise. Unfortunately, these PET scans are very expensive, slightly invasive, and often times not covered by insurance, including Medicare. Establishing a blood test to detect at risk individuals is urgent. Numerous research groups have been working towards this goal with one test, by the company Shimadzu Corp, being 88% accurate at identifying those at risk. Early detection of the disease is necessary as we have learned that anti-amyloid drugs do not work in individuals with prodromal or full-blown Alzheimer’s disease.
There are few treatment options currently available, drugs like Aricept and Namenda, only successfully treat symptoms in a minority of patients. There is no cure for Alzheimer’s disease. The need for a disease modifying agent to combat Alzheimer’s disease is growing. New drugs are being tested to halt the progression or prevent the initiation of the disease. The most common targets for these drugs are amyloid protein, tau protein, and the brain inflammation these mis-folded proteins cause.
A change has recently occurred within Alzheimer’s disease research. The lack of efficacy of anti-amyloid drugs in people with symptoms has motivated researchers to target factors other than amyloid, such as the mis-folded tau protein, and brain inflammation. Our fight against Alzheimer’s disease continues at the Center for Cognitive Health as we continue to work within the global research community seeking the first ever FDA-approved disease modifying medication for Alzheimer’s disease.
