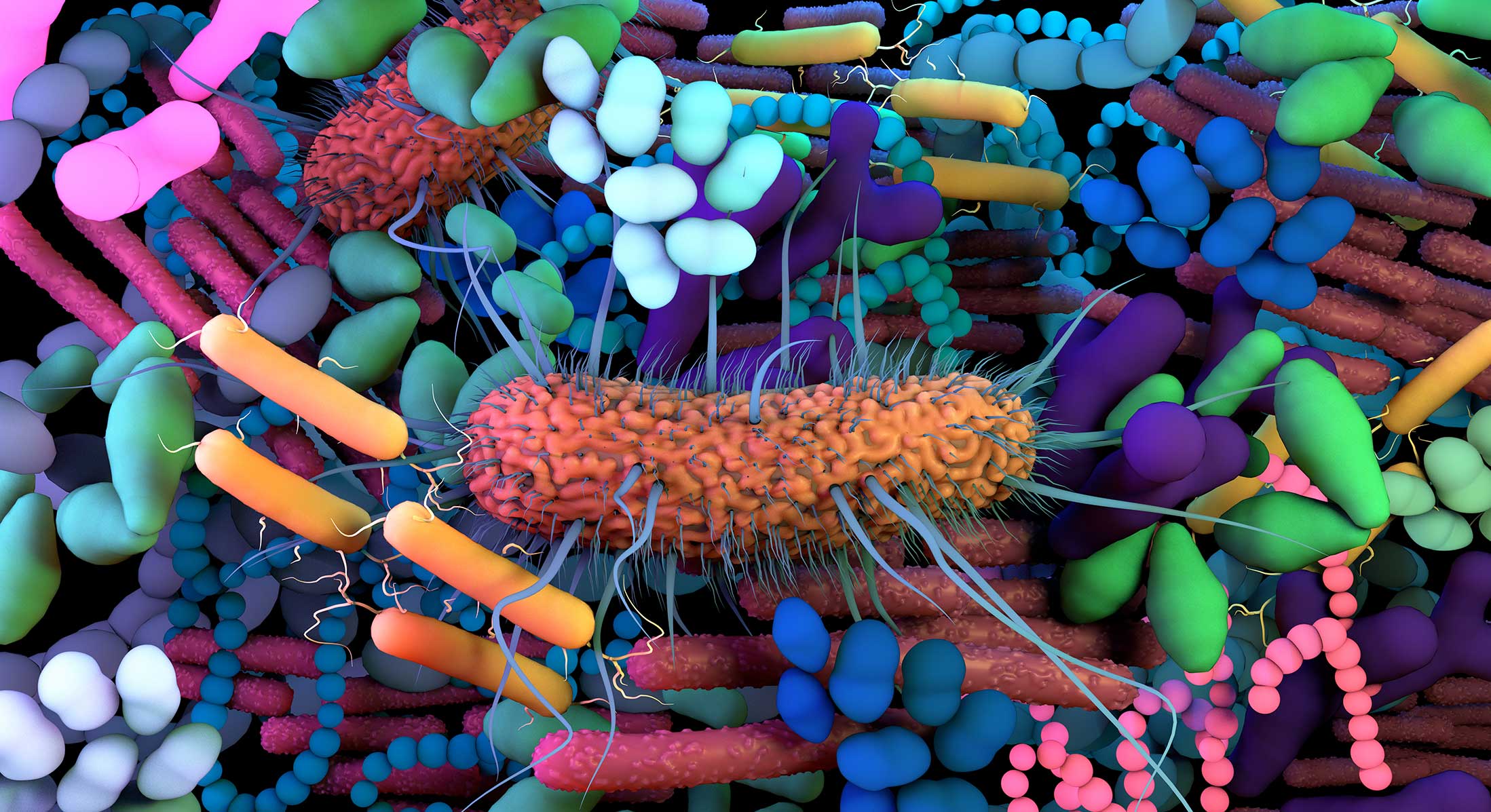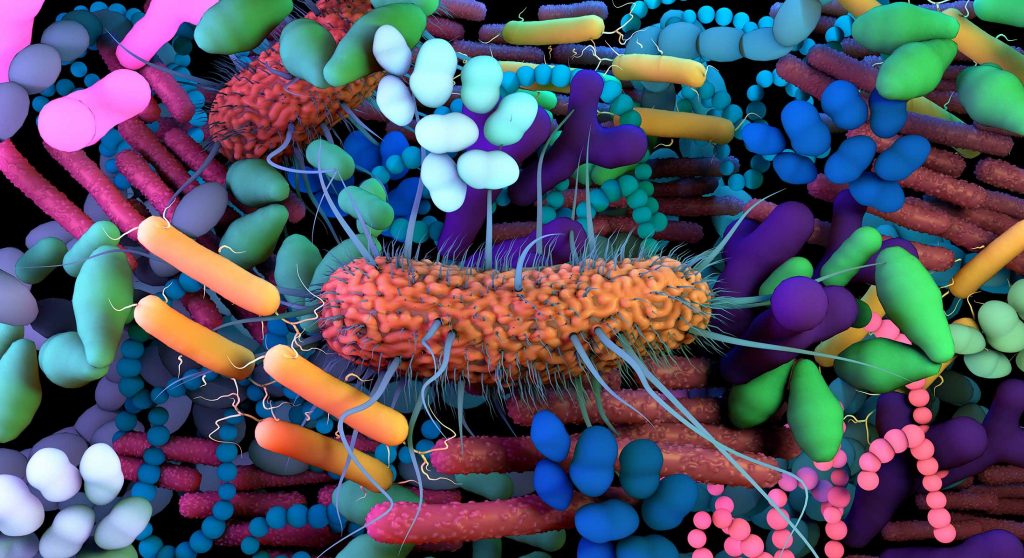
We each have a unique and complex network of microbes living within our guts known as a microbiome. It is comprised of a dynamic ecosystem of viruses, fungi, and predominately bacteria. As humans, we have been evolving and diversifying in concert with our microbiomes for at least 15 million years, indicating a close bacteria-host mutualism. Colonization of your gut microbiome occurs during birth, is highly dynamic throughout infancy, and resembles adult microbiomes in approximately three years remaining stable thereafter. Several factors influence the microbiome, such as genetics, diet, metabolism, age, geography, stress, antibiotic treatment, probiotics, disease, and more. Microbes within the microbiome are responsible for extracting energy from the food we eat, vitamin biosynthesis, pathogen overgrowth protection, educating our immune system, and more.
Alterations in the gut microbiome are associated with an array of metabolic and gastrointestinal diseases like irritable bowel syndrome (IBS) and insulin resistance, but recent research has found that other body regions are also affected. Your gut microbiome is important and key in regulating digestion, hormones, immunity, the brain and cognition. Due to this newly established relationship between the central nervous system (CNS) and our gut microbiomes a circular communication loop, often referred to as the gut-brain axis, has been established. The loop is bidirectional with disruption at one end of the axis often instigating a dysregulation in the other. Changes to the gut microbiome have recently been associated with neurodegenerative diseases like Parkinson’s disease, multiple sclerosis, and Alzheimer’s disease (AD).
Recent studies performed in mice suggest that alterations in the gut microbiome contribute to amyloid plaque deposition in AD. AD mice treated with long-term broad-spectrum antibiotics (to significantly alter their microbiome population) result in less amyloid plaque deposition with higher circulating soluble amyloid levels compared to untreated AD mice. Analyses of the AD mouse microbiome revealed decreased microbial diversity in treated mice with reduced Firmicutes and Bifidobacterium bacteria, but increased Bacteroidetes bacteria compared to untreated mice. Additionally, although the balance of microbiome components changed, the total abundance of the population remained similar to pre-antibiotic treatment. These findings suggest that the gut microbiome diversity plays a role in regulating individual amyloid plaque development, or amyloidosis.
Based on animal studies, diet and physical exercise also effect the gut microbiome resulting in further downstream effects on cognition. Mice consuming a high fat diet (HFD) compared to a normal diet (ND) restructure their gut microbiomes resulting in increased anxiety. Exercise was shown to alter the microbiomes of both groups to similar magnitudes regardless of diet. Although exercise slightly improved memory in HFD mice, it could not quell their increased anxiety, indicating that exercise cannot counteract all effects of a poor diet. Exercised ND mice show increased memory and learning and result in increased Firmicutes bacterial strains when compared to ND mice without exercise. Diets high in fat and exercise both have the ability to alter the gut microbiome and behavior, but independently.
Mice with reduced microbiomes from birth result in modified development of two particular brain regions, the amygdala and hippocampus. Signaling between the amygdala and hippocampus modulates social behaviors and anxiety, and alterations in their development may lead to disrupted behaviors. Both regions enlarged in germ free (GF) mice, but total brain volume remained similar to normal germ (NG) mice. The amygdala appeared to be hyperactive in GF mice with an underactive hippocampus compared to NG mice. GF mice have an increased stress response compared to NG mice. This research indicates that an appropriately populated microbiome is necessary for normal brain development and neural communication and might prevent the development of mental illness like depression and anxiety.
The brains of animals with modified or absent microbiomes display a variety of molecular differences, like varied expressions of neurotransmitters and their receptors when compared to
animals with unaltered microbiomes. Reductions in brain-derived neurotrophic factor (BDNF) gene expression occurs in GF mice compared to NG mice, primarily in the hippocampus. BDNF is important for neuronal survival and growth, and learning and memory. Inhibitory neurotransmitter effects were lower in the hippocampus and amygdala of mice that ingested L. rhamnosus bacteria as a probiotic compared to those untreated. These same mice display reduced anxiety- and depression-related behavior. This not only emphasizes that our microbiome effectsour cognition, but that we can purposefully manipulate it. If we can learn more about the gut-brain axis and determine which microbes are beneficial we could use them as viable treatments.
It’s becoming more and more clear that our microbiomes greatly influence our bodies, including the brain, but what about the effects our brains may have on our microbiomes? Do we possess the ability to modify our microbiomes to serve our bodies better? Tune in next week for part two in the three part series that is: “The Gut-Brain Axis”!!