Clinical neurodegenerative research is at an exciting crossroads. Scientists and pharmaceutical companies are focusing on a variety of innovative approaches to better understand and treat theses complex diseases, including Alzheimer’s disease (AD), Lewy body dementia (LBD), and Parkinson’s disease (PD). Emerging trials are exploring novel therapies targeting not only symptom management but also disease origination.
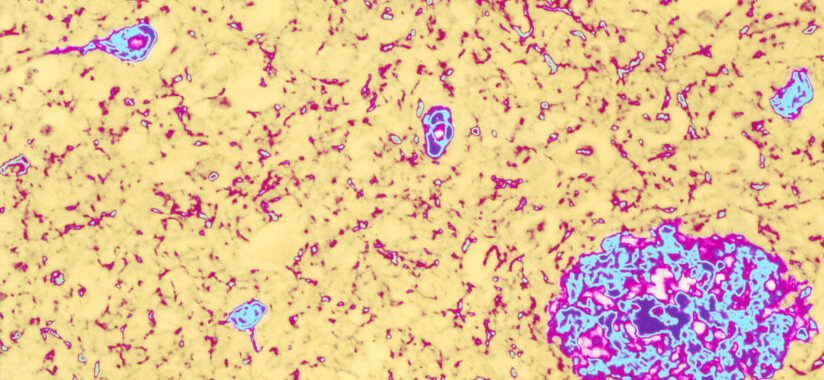
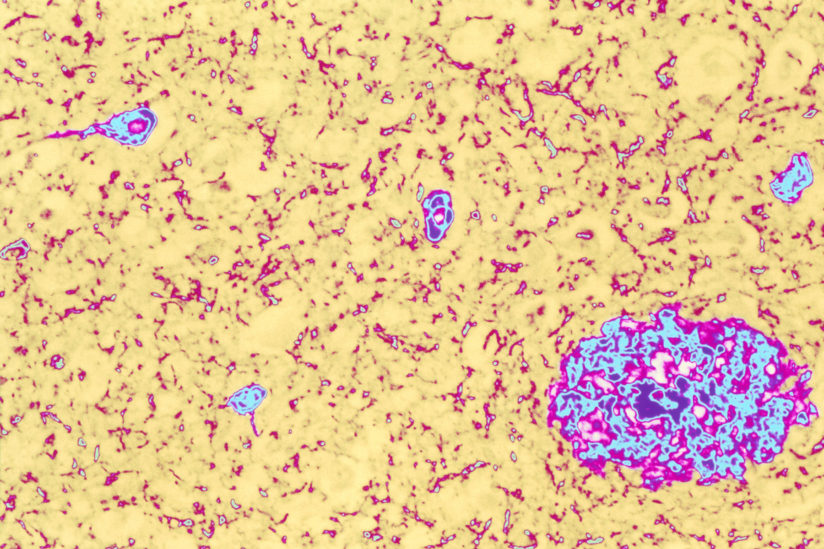
At the heart of AriBio’s AR1001 investigational drug’s potential lies its groundbreaking mechanism of action. The oral drug seeks to target the underlying factors responsible for AD, in hopes of slowing down or even halting disease progression. Although first established for erectile dysfunction, AR1001 appears to reduce amyloid b (Ab) protein and increase blood flow in the brain. It’s accomplished via a selective phosphodiesterase 5 inhibitor preventing degradation of secondary messengers (cAMP and cGMP) regulating cellular functioning. By reducing neuroinflammation, promoting neural regeneration, and mitigating the toxic Ab plaque build-up in the brain, AR1001 represents a potential leap forward in AD treatment.
Cognito Therapeutics’ CA-0011 trial showcases a novel route to combat AD. It combines elements of neuroinflammation reduction, neural regeneration promotion, and the mitigation of Ab plaques in the brain. Their innovative investigational device utilizes non-invasive neuromodulation techniques to target specific brain regions associated with cognitive function, achieved by delivering 40Hz gamma stimulation through a self-administered glasses headset. By providing precisely tuned electrical currents, the device aims to modulate neural activity, enhance synaptic plasticity, and promote neural connectivity in a region-specific manner. This neuromodulation approach is designed to optimize brain function and potentially ameliorate cognitive deficits. The device’s non-invasive mechanism of action represents a promising avenue in the quest for effective treatments and cognitive improvements for patients suffering from AD.
Eli Lilly continues to produce evermore promising monoclonal antibodies targeting AD, with one of the newest being Remternetug. These antibodies bind to Ab plaques in the brain, initiating immune cells, or microglia, to clear them. Following in the footsteps of Donanemab, this investigational drug also targets the pyroglutamated structure of Ab in plaque form, but it’s given as a simple injection rather than an IV-infusion. When Remternetug was given to AD patients for 6 months, around 75% resulted in Ab plaque clearance. That took Donanemab 18 months to do, suggesting Remternetug may be a more sufficient therapeutic.
Neflamapimod, developed by EIP Pharma, is a small molecule investigational drug showing promise for a multitude of neurodegenerative diseases. It’s designed to inhibit the enzyme p38 MAP kinase targeting the cholinergic system, believed to be involved in the inflammation and cell dysfunction and death associated with PD, LBD, and AD. By targeting these pathways Neflamapimod’s goal is to reduce neuroinflammation, alleviate some motor symptoms, and potentially slow down cognitive decline. It appears to work best in those with low baseline ptau181 levels and less extensive cortical neurodegeneration. When tested in AD patients, those with ptau181 levels below 2.2 ng/mL resulted in substantial benefits to attention, dementia severity, motor functional mobility, and memory compared to those with higher levels of the biomarker. A similar pattern is seen with DLB patients with normal ptau181 levels improving compared to those with abnormally elevated levels. Based on these findings, a criterion limiting those with higher ptau181 levels could uncover a greater efficacy for those on Neflamipimod to treat DLB. A phase IIb clinical trial, RewinD-LB, is ongoing to evaluate its safety and efficacy, offering optimism for a new therapeutic approach for DLB.
These promising developments bring new hope for improved care and potentially disease-modifying treatments. While there is still much to learn and discover, the field of neurodegenerative disease research is advancing, inching closer to a future with effective interventions and even potential cures. If you, or anyone you know, may be interested in taking part in a clinical trial involving any of the above discussed investigational therapeutics, please reach out to us at 503-548-0908.
Sources:
Alam, John, et al. “Association of Plasma Phosphorylated Tau with the Response to Neflamapimod Treatment in Patients with Dementia with Lewy Bodies.” Neurology, 1 Sept. 2023, pp. 10.1212/WNL.0000000000207755–10.1212/WNL.0000000000207755, https://doi.org/10.1212/wnl.0000000000207755. Accessed 31 Oct. 2023.
“AR1001 | ALZFORUM.” Www.alzforum.org, 10 Mar. 2023, www.alzforum.org/therapeutics/ar1001. Accessed 31 Oct. 2023.
Beaney, Abigail. “First Patient Dosed in Phase IIb RewinD-LB Trial for DLB.” Clinical Trials Arena, 14 Aug. 2023, www.clinicaltrialsarena.com/news/neflamapimod-trial-dementia-lewy-bodies/?cf-view. Accessed 31 Oct. 2023.
Benussi, Alberto, et al. “Exposure to Gamma TACS in Alzheimer’s Disease: A Randomized, Double-Blind, Sham-Controlled, Crossover, Pilot Study.” Brain Stimulation, vol. 14, no. 3, May 2021, pp. 531–540, https://doi.org/10.1016/j.brs.2021.03.007.
“Cognito Therapeutics Announces Proprietary Gamma Sensory Stimulation for 6-Months Reduces White Matter Atrophy in Alzheimer’s Disease Patients.” Www.businesswire.com, 1 Aug. 2022, www.businesswire.com/news/home/20220801005207/en/Cognito-Therapeutics-Announces-Proprietary-Gamma-Sensory-Stimulation-for-6-Months-Reduces-White-Matter-Atrophy-in-Alzheimer%E2%80%99s-Disease-Patients.
Senior, Emily Craig. “Another Alzheimer’s Drug Could Be Better than Donanemab.” Mail Online, 19 July 2023, www.dailymail.co.uk/health/article-12314599/Another-Alzheimers-drug-pipeline-looks-better-donanemab.html. Accessed 31 Oct. 2023.
“Treatment Effect of Neflamapimod Enriched When Excluding High P-Tau181 Level Patients.” Neurology Live, 11 Sept. 2023, www.neurologylive.com/view/treatment-effect-neflamapimod-enriched-excluding-high-p-tau181-level-patients. Accessed 31 Oct. 2023.